CommentsGUEST WORDS-You often compare our economy to those of other countries, proud to say that California boasts the fifth largest in the world.
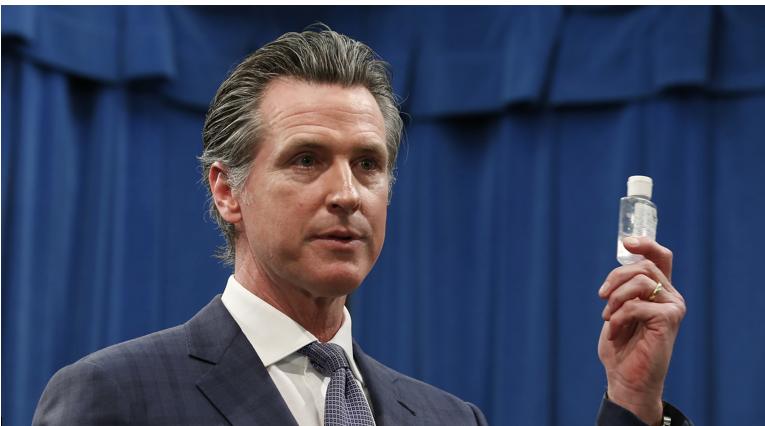
If the appropriate scale of comparison is country to California, and not state to state, then we need country-like leadership. And this leadership must come from you. We need an authoritative, coordinated response, with our governor in charge of the messaging, to explain clearly how he will keep Californians safe.
I believe the current approach of devolving the leadership of the COVID-19 response to the county level is ill advised. This devolution may lead to mixed messages, divergent containment approaches, and different treatment outcomes, depending on geography. Work with county public health officials, and facilitate coordination among counties and cities, but come up with a uniform set of guidelines for the entire state and push clear messages to the public now. We need our governor to take the lead. People have become confused, in no small part because of the lack of leadership and clarity coming from the White House and viral social media posts.
County-level public health officials have an enormous job of protecting the health of thousands or millions of people. We need them to stay the course. In LA, Barbara Ferrer has been in the public eye doing a good job of communicating important information clearly, but it is not getting out to most Angelenos, perhaps because most do not know where to look for it or do not consume the forms of media that broadcast her press briefings.
We need messaging by a single leader disseminated widely over every media platform and in multiple languages. The face of our governor should be the one we look to when hearing for the validated measures that have worked in South Korea: aggressive social distancing and containment, and quarantines when community outbreaks have been verified. Testing should be widespread and performed in every community. South Korea has managed to test 10,000 people a day. California should also have this capacity. The push for social distancing should be loud and bold. You must craft messages that motivate people to think of their whole communities, not just themselves.
Peer-reviewed research on SARS-CoV-2 and its resulting illness, COVID-19, is published every week. Many medical professionals who have had firsthand experience treating COVID-19 patients have sounded the alarm, urging the United States to mount a more robust response to this deadly illness. The World Health Organization (WHO) declared a pandemic on Wednesday morning and emphasized that containment should be the “major pillar” of response to this viral outbreak. It is not too late for California to adopt more aggressive measures.
In California the number of infected people rises daily, but without vastly expanded testing, we cannot understand the extent of the virus’s spread. I urge you to ramp up the number of tests rapidly.
COVID-19 is more infectious than the flu, according to reputable sources and the WHO. One WHO spokesperson at Wednesday morning’s press conference stated, “This is not the flu.” A person ill with the flu infects on average 1.3 persons. In contrast, a person ill with COVID-19 infects two to four persons. Moreover, a study published this week on bus passengers in China found that one person with symptoms infected seven people on his four-hour bus ride; his infected droplets distributed through coughing and sneezing stayed airborne for 30 minutes, infecting four more people on the subsequent bus ride after he and his co-passengers had disembarked. People wearing masks on the initial bus ride did not contract the virus from him.
Los Angeles Will Likely Need State Support Coping with the Outbreak
Los Angeles will need more hospital beds and medical supplies than it currently has. Last fall I accompanied a family member to the emergency room at Ronald Reagan-UCLA Medical Center on an ordinary weekday. We had to wait three hours before he could be seen by a physician. When a nurse took us back to the ER, we walked through double doors into a bustling, chaotic theater of patients and medical personnel. We walked past patients in wheelchairs, on gurneys, and on examination tables. We walked past the crowded central workstation teeming with nurses, doctors, and staff, down a corridor, through double doors, and into another hallway to a makeshift patient-holding area, filled with exam tables, partitions, rolling carts, and patients and doctors.
We overheard doctors refer to this improvised section as “Narnia.” One doctor speaking to another on the phone said, “I’m in Narnia.” On an ordinary weekday in Los Angeles before the flu season had begun, the ER was bursting at the seams, and UCLA doctors had an established overflow area called Narnia. What will LA do when the full impact of the novel coronavirus hits? Where will the overflow treatment areas be situated?
The risk of severe illness after contracting the novel coronavirus increases after the age of 9, unless children have underlying chronic medical conditions. Particularly vulnerable people are those suffering from obesity, diabetes, cancer, respiratory illnesses, and other preexisting medical conditions. Data on COVID-19 has demonstrated consistently that people over the age of 70 are at significantly greater risk of death. But in the Golden State, arguably one of the most vulnerable populations to contracting the novel coronavirus comprises unsheltered members of our communities subsisting in tent encampments, on sidewalks, under freeway overpasses, in flood-control basins, and in brushy areas. What leadership do you offer to protect and safeguard the health of homeless Californians right now, today? How will you act to prevent COVID-19 outbreaks in encampments and among homeless individuals?
We look to elected officials to lead. Correct advice is not reaching the average Californian. People are confused. Many still say that the novel coronavirus is like the flu and there is no need to worry. It is, however, far more lethal, leading to hospitalization for 10% to 20% of those infected by it, with a death rate (the lower estimate is 1%) at least 10 times greater than that of flu (0.1%); if the figure published by the World Health Organization is accurate (3.4%), the mortality rate for COVID-19 is 34 times greater than that of flu.
If the spread of the virus is not checked through swift and assertive containment methods, including social distancing and contact tracing, self-isolation, and when necessary, quarantines, then the sickest patients will need intensive medical care at the same time, which will overwhelm our hospitals. This scenario is playing out in Italy right now. The worst cases have peaked together, and the healthcare system could not handle it. We need to flatten the curve by stanching the spread of the virus. We want to do everything we can to avoid a sharp peak in demand for the most intensive medical services and devices. Quarantines and social distancing need to begin as soon as the evidence of community spread in given neighborhoods or communities is known. But we cannot know that until we have more testing.
In the meantime, Governor Newsom, communicate with Californians directly. The virus knows no geographic boundaries. It will not know when it has crossed from one city or county to another. We need clear guidance. We need to be inspired to think of each other, to change our behaviors for the greater good.
Otherwise, in three to four weeks Italy will be our future.
(Gina K. Thornburg, PhD, is the Executive Director of Coalition for Valley Neighborhoods based in Woodland Hills. A housing-, environmental-, and social-justice activist and advocate. She is the at-large alternate board member of the Woodland Hills-Warner Center Neighborhood Council, is a founding member of the West Valley Neighborhood Alliance on Homelessness, and sits on the board of United Neighborhoods 4 LA. She may be reached at [email protected].) Prepped for CityWatch by Linda Abrams.